Five Scars or One? The Question That Reveals Everything About Your Surgeon
Count the incisions.
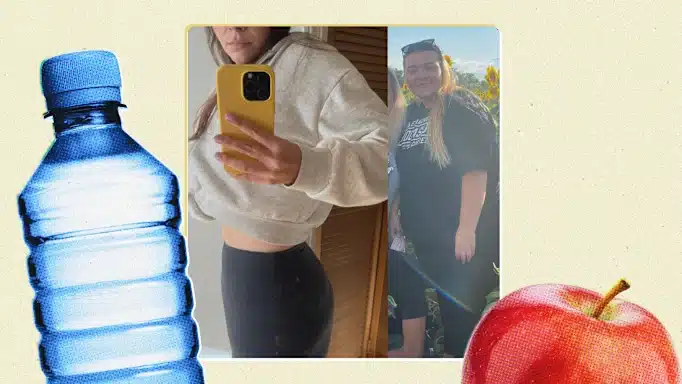
That’s what I tell patients when they’re comparing bariatric surgeons. Not the price. Not the flashy website. Not even the before-and-after photos (those can be cherry-picked). Count the incisions the surgeon typically uses.
A standard laparoscopic gastric sleeve requires five to seven small incisions across your abdomen. Each incision is a port, an entry point for camera and instruments. Each port means a separate puncture through your skin, fat layer, fascia, and muscle. Each puncture creates inflammation. Each one leaves a scar.
But there’s another way.
Single-incision laparoscopic surgery (SILS) accomplishes the entire operation through ONE incision, hidden inside your belly button. When healed, most patients have zero visible scars. The surgery happened, the weight comes off, but the evidence disappears inside your navel.
Now here’s what most surgeons won’t tell you: the reason THEY don’t offer single-incision surgery isn’t patient selection or medical indication. It’s skill.
Operating through a single port is exponentially more difficult than multiport surgery. The instruments crowd each other. The angles are awkward. The visualization is limited. The margin for error shrinks to nearly zero.
I offer single-incision gastric sleeve because I can. After 7,800+ surgeries and a PhD that trained me to understand tissue at the molecular level, I have the technical precision to operate through a space most surgeons would consider impossible.
And that precision doesn’t just mean fewer scars. It means less internal trauma, lower inflammatory response, and faster recovery.
Let me explain everything.
What Exactly Is Single-Incision Gastric Sleeve Surgery?
Single-incision laparoscopic sleeve gastrectomy (SILSG) is the same Enhanced Gastric Sleeve procedure performed through a single 2-3cm incision concealed within the umbilicus, rather than the traditional five to seven separate incisions distributed across the abdomen. The surgical outcome is identical. The weight loss is identical. The only difference is HOW the surgeon accesses the surgical field.
Think of it this way: imagine you need to renovate a room in your house. One contractor says they need to knock five holes in your wall to get their tools inside. Another contractor can do the same job through one opening they’ll patch so perfectly you’ll never know it was there.
Same renovation. Same result. Vastly different skill requirements.
The Technical Reality
During a standard multiport gastric sleeve, I would typically place:
- One 12mm port at the umbilicus (camera)
- One 12mm port in the left upper abdomen (stapler)
- One 5mm port in the left flank (liver retractor)
- One 5mm port in the right upper abdomen (grasper)
- One 5mm port (optional) for additional retraction
Each of these ports gives my instruments room to move independently. I have triangulation, meaning my instruments approach the surgical field from different angles like points of a triangle. This is standard laparoscopic technique taught in every surgical residency.
During single-incision surgery, I accomplish ALL of this through ONE opening:
- Camera, stapler, graspers, liver retractor, all entering through the same 2-3cm umbilical incision
- Specialized ports (like the GelPoint device) allow multiple instruments through a single fascial defect
- Articulating instruments bend at angles to recreate triangulation from a single access point
- The liver must be retracted using suture techniques rather than an external port
The difficulty increases by an order of magnitude. My instruments are fighting for the same space. My angles are compromised. I’m operating with my hands essentially crossing over each other.
Why would any surgeon choose this harder path?
Because when you CAN do it, the benefits for the patient are significant.
The Research: What Science Says About Single-Incision Bariatric Surgery
I don’t ask patients to trust marketing claims. I ask them to trust data. Here’s what the published research demonstrates:
Pain Reduction
A randomized controlled trial comparing single-port to multiport sleeve gastrectomy found that single-incision patients reported significantly lower pain scores on postoperative days 1 and 2.
Specifically:
- Day 1: Single-incision 34.1 VAS vs. Multiport 49.3 VAS (p = 0.046)
- Day 2: Single-incision 22.1 VAS vs. Multiport 35.9 VAS (p = 0.044)
By day 3, the difference normalized. But those first 48 hours are when pain is most intense, when patients struggle to walk, when recovery feels overwhelming. Reducing that acute pain window matters.
Cosmetic Satisfaction
A 2020 meta-analysis in Obesity Surgery examined 11 studies with 1,168 patients comparing single-incision to conventional laparoscopic sleeve gastrectomy. The findings:
Patients in the SILS group reported 2.47 times greater satisfaction with cosmetic scar outcomes (SMD = 2.47, 95% CI = 1.10 to 3.83, P = 0.00).
A 2-year prospective study of 600 patients by Lakdawala et al. used a specific “scar satisfaction score” and found the single-port group displayed significantly higher satisfaction.
Some surgeons dismiss cosmetic outcomes as vanity. I disagree. Approximately 70% of bariatric surgery patients are women. Many have spent years feeling self-conscious about their bodies. Many have hidden their weight struggles from friends, family, even themselves. The idea that their surgery could remain invisible, that they could reveal their transformation on their own terms without visible surgical scars, carries genuine psychological value.
Equivalent Weight Loss
Critics initially questioned whether single-incision surgery might compromise weight loss outcomes. The data has answered definitively: no difference in weight loss or comorbidity resolution between SILS and conventional laparoscopic sleeve gastrectomy.
The 2020 meta-analysis found no significant differences in:
- Operative time
- Intraoperative estimated blood loss
- Conversion rate
- Intraoperative complications
- Length of hospital stay
- Postoperative analgesia requirements
- Postoperative complications
- Excess weight loss (EWL)
- Improvements in comorbidities (P > 0.05 for all)
Same results. Less pain. Better cosmesis. The only “cost” is requiring a surgeon with advanced skills.
Safety Profile
A 2017 review in the Journal of Laparoendoscopic & Advanced Surgical Techniques analyzed 19 studies comprising 1,679 patients who underwent single-incision laparoscopic sleeve gastrectomy.
Their conclusion: “SILSG is safe and feasible.”
A 2025 meta-analysis examining port-site complications across 40,248 laparoscopic patients found that bariatric surgeries had the LOWEST incidence of port-site hernia at just 0.57%, compared to 1.47% for colorectal surgeries.
A 2024 comprehensive review in PMC documented post-laparoscopic complication rates:
- Gastrointestinal: 0.6 per 1,000
- Genitourinary: 0.3 per 1,000
- Vascular: 0.1 per 1,000
- Omentum: 0.4 per 1,000
These rates apply regardless of single-incision or multiport approach. The surgical procedure itself, not the access method, determines most complication risks.
The Comparison: Standard Sleeve vs. Single-Incision Sleeve
| Factor | Standard 5-Port Sleeve | Single-Incision Sleeve |
|---|---|---|
| Number of Incisions | 5-7 separate incisions | 1 incision hidden in belly button |
| Visible Scars | 5-7 small scars across abdomen | Zero visible scars when healed |
| Postop Pain Day 1 | VAS ~49 | VAS ~34 (30% less) |
| Postop Pain Day 2 | VAS ~36 | VAS ~22 (39% less) |
| Weight Loss at 6mo | Identical | Identical |
| Complication Rate | Identical | Identical |
| Operative Time | ~60-90 minutes | ~85-100 minutes |
| Surgeon Skill Required | Standard laparoscopic | Advanced (SILS-certified) |
| Patient Selection | All candidates | BMI <50, favorable anatomy |
| Cosmetic Satisfaction | Good | 2.47x higher |
| Port-Site Hernia Risk | 0.57% (distributed across ports) | 0.57% (concentrated at umbilicus) |
| Recovery to Work | 7-10 days | 7-10 days |
| Cost (Dr. Gabriela) | $5,000-$7,000 | $5,000-$7,000 |
The key insight: surgical outcomes are equivalent, but the patient experience differs meaningfully in pain and cosmetic results.
Why Most Surgeons Don’t Offer Single-Incision: The Honest Answer
Here’s the uncomfortable truth the bariatric industry doesn’t discuss openly.
Single-incision surgery is harder. It takes longer to learn, requires more expensive specialized instruments, increases operative time slightly, and carries no additional reimbursement from insurance. From a pure business standpoint, it’s inefficient.
A surgeon can complete more five-port procedures in a day than single-incision procedures. Each surgery generates similar revenue. The financial incentive is to go faster, not more precise.
Additionally, the learning curve is significant. Published literature describes single-incision bariatric surgery as requiring “confident, multiport laparoscopic skills” as a prerequisite. One technical review noted: “This procedure requires far more skill than conventional laparoscopic multiport surgery and should only be undertaken by SILS and bariatric experienced surgeons.”
I offer single-incision surgery for patients who are good candidates because I believe you deserve access to the best technique available, not the easiest one for me.
My training prepared me for this. My PhD research involved years of precise laboratory work where millimeters matter. My 7,800+ surgeries built muscle memory. My drainless technique already demonstrates the surgical precision required for SILS.
When you come to me for an Enhanced Gastric Sleeve, we’ll discuss whether you’re a candidate for single-incision. Not every patient is. But if your anatomy is favorable and your BMI allows it, I can offer you this option because I have the skills to execute it safely.
Patient Selection: Who Is a Candidate for Single-Incision Gastric Sleeve?
Single-incision gastric sleeve is ideal for patients with BMI below 50, favorable abdominal anatomy, no prior upper abdominal surgeries, and appropriate xiphoid-to-umbilicus distance. Not every patient qualifies, and honest assessment is critical for safe outcomes.
Ideal Candidates
Based on published criteria and my clinical experience, the best candidates for SILS gastric sleeve include:
- BMI 35-50: Higher BMI increases technical difficulty and may compromise safety
- Female patients: Generally have more favorable anatomy for umbilical access (shorter torso, less intra-abdominal fat)
- No prior upper abdominal surgery: Previous surgery creates adhesions that complicate single-port access
- Xiphoid-to-umbilicus distance <25cm: Longer distances make instrument reach difficult
- No large hiatal hernia requiring extensive repair: Some hiatal hernia repair is possible through single incision, but complex repairs may require additional ports
- No severe hepatomegaly: Enlarged liver makes retraction challenging through limited access
Patients Who May Need Multiport Approach
Some patients are better served by traditional five-port laparoscopy:
- BMI >50: The technical difficulty and safety margin favor multiport access
- Prior upper abdominal surgery: Adhesions require careful lysis that benefits from triangulation
- Significant hepatomegaly: Large, fatty liver needs robust retraction
- Complex hiatal hernia: Extensive repair requires optimal visualization
- Very tall patients (>180cm): Instrument reach becomes limiting
- Central obesity pattern: Thick omentum and short mesentery complicate single-port work
My Approach
During your virtual consultation, I review your measurements, medical history, and imaging (if available). I’m completely honest about which approach I recommend.
I would rather tell you that you need a five-port procedure than attempt single-incision surgery on an unsuitable candidate. Your safety comes first. Always.
If I determine you’re a candidate for single-incision, I explain both options and let you choose. Some patients prefer the certainty of conventional multiport even when SILS is feasible. That’s perfectly valid. It’s your body, your surgery, your decision.
The Technical Details: How I Actually Perform Single-Incision Sleeve Gastrectomy
For patients (and referring physicians) who want to understand the specific technique, here’s how I approach single-incision gastric sleeve:
Pre-Operative Setup
- Patient positioning: supine with legs split on a bean bag
- Surgeon stands between patient’s legs (French position)
- Assistant on patient’s right
- Camera holder on patient’s left
The Umbilical Incision
I create a 2-3cm vertical incision through the umbilical folds. The umbilicus is the thinnest point of the abdominal wall, providing the easiest access with the least tissue trauma. Crucially, the final scar hides within the natural umbilical creases.
The incision extends through:
- Skin
- Subcutaneous fat
- Fascia (linea alba)
- Peritoneum
Port Placement
I use a specialized access device (GelPoint or similar) that allows placement of multiple trocars through a single fascial opening. This device creates an airtight seal maintaining pneumoperitoneum while accommodating:
- 10mm camera port
- Two 5mm working ports
- Smoke evacuation
Liver Retraction
This is the critical step that differentiates experienced SILS surgeons.
In multiport surgery, a dedicated liver retractor enters through a separate left-flank port. In single-incision, I must retract the liver using alternative techniques:
Suture suspension method: I place a suture through the falciform ligament and bring it out through the abdominal wall, elevating the left lobe of the liver. This provides stable retraction without an additional port.
Some surgeons use specialized internal retractors, but I prefer the suture method for its reliability and minimal additional trauma.
Gastric Dissection and Stapling
Using articulating instruments that bend at angles to recreate triangulation, I:
- Divide the gastrocolic ligament starting 2-4cm from pylorus
- Mobilize the greater curvature to the angle of His
- Identify and preserve the gastroepiploic vessels
- Calibrate with a 36-40 French bougie
- Sequential stapling from antrum to fundus using articulating endostaplers
- Apply my staple line reinforcement technique (Seamguard + oversewing)
- Perform leak test
Hiatal Hernia Assessment
I routinely inspect the hiatal region. If a hiatal hernia is present, I repair it as part of my acid reflux prevention protocol. Small hernias can be addressed through single incision. Large hernias may require an additional 5mm port for optimal repair.
Specimen Extraction
The resected stomach portion extracts through the umbilical incision, which is already large enough to accommodate the specimen without extension.
Fascial Closure
This is CRITICAL for preventing port-site hernia. Because the umbilical incision is larger than standard trocar sites, meticulous fascial closure with absorbable sutures is mandatory. I close the fascia in layers to ensure strength.
Skin Closure
Absorbable subcuticular sutures close the skin. The final incision hides within the umbilical folds. Most patients cannot identify their surgical incision once fully healed.
My Enhanced Protocol: Single-Incision PLUS Safety Features
Let me be direct: the single incision is just the access method. What I do INSIDE your abdomen is what determines your outcome.
When I perform single-incision gastric sleeve, I include ALL elements of my Enhanced Protocol:
1. Triple-Layer Staple Line Protection
- Seamguard reinforcement material along the entire staple line
- Invaginating (oversewing) sutures burying the staple line
- Meticulous hemostasis preventing any bleeding that could compromise healing
Result: My leak rate approaches zero. Bleeding complications are virtually eliminated.
2. Hiatal Hernia Repair
I actively inspect and repair any hiatal hernia encountered. This is NOT standard at many clinics, particularly high-volume “factory” operations that prioritize speed.
Result: Dramatically reduced long-term acid reflux, the most common complaint after standard sleeve gastrectomy.
3. TAP Block Pain Management
My Transversus Abdominis Plane Block injects long-acting local anesthetic into the abdominal muscle layers DURING surgery. Combined with the reduced trauma of single-incision access, patients experience remarkably manageable postoperative pain.
Result: Most patients walk within 3 hours. Opioid use is minimal. Nausea is reduced.
4. Drainless Technique
My surgical precision allows me to perform drain-free surgery. No tubes, no bulbs, no painful removal, no drain-site scars.
With single-incision surgery PLUS drainless technique, patients have literally ONE small incision that heals invisibly inside their belly button. The transformation happens without visible evidence.
What Patients Actually Experience: Recovery Timeline
Let me walk you through what to expect after single-incision gastric sleeve with my Enhanced Protocol:
Day of Surgery
- Surgery duration: 85-100 minutes
- Awaken in recovery with numb abdomen (TAP Block effect)
- Walking within 3 hours
- Clear liquids begin same day
- One night hospital stay at our QUAD A accredited facility
Day 1
- Discharge to recovery hotel
- Mild discomfort, well-controlled with oral medication
- Walking encouraged every 2 hours
- Liquid diet continues
- My team checks on you in person
Days 2-3
- Most patients feel “surprisingly good”
- Pain levels significantly lower than expected
- Walking comfortably, albeit slowly
- Sipping liquids, transitioning to protein shakes
- Typical return travel home (if flying from US)
Day 4
- Activity restrictions: no lifting >10 lbs
- Continue liquid/soft protein diet
Week 1
- Most patients return to sedentary work (desk jobs, remote work)
- Mild fatigue is normal as body adjusts
- Daily walking encouraged
Week 2-3
- Energy improving
- Transition to pureed foods
- Light activity resumes
Week 4
- Soft foods introduced
- Return to normal activity for most patients
- Exercise (walking, light cardio) can increase
Week 6+
- Regular food introduction (small portions)
- Full activity including exercise
- Weight loss accelerating
The Scar
- Weeks 1-2: Incision may appear pink, slightly raised within umbilicus
- Weeks 3-6: Gradual fading
- Months 3-6: Most patients cannot identify the incision
- 1 Year: Essentially invisible for most patients
The Real Questions Patients Ask Me
After 7,800+ surgeries, I’ve heard every question. Here are the honest answers to what patients really want to know:
“Is single-incision surgery riskier?”
No. The research shows equivalent complication rates between single-incision and multiport approaches. Both are safe when performed by experienced surgeons. The key word is “experienced.” Single-incision surgery in the hands of an inexperienced surgeon IS riskier. That’s why patient selection and surgeon qualifications matter.
“Why doesn’t my local surgeon offer this?”
Probably because they haven’t invested in the specialized training and equipment. Single-incision surgery requires articulating instruments, specialized access ports, and hours of additional training. Many surgeons don’t see the value since insurance reimbursement is identical. Their loss, potentially your gain.
“Will my insurance cover single-incision?”
If your insurance covers gastric sleeve surgery, it typically covers single-incision gastric sleeve at the same rate. The surgical codes are equivalent. However, since I practice in Mexico, this is generally a self-pay question for my US patients. My Enhanced Gastric Sleeve at $5,000-$7,000 is already a fraction of US costs ($20,000+), and single-incision is included at no additional charge for suitable candidates.
“What if you can’t complete the surgery through one incision?”
This is called “conversion,” and it’s a sign of good judgment, not failure. If I encounter unexpected adhesions, bleeding, or anatomical challenges that compromise safety, I add one or more ports without hesitation. Your safety trumps cosmetic outcomes every time. In my experience, conversion rates for appropriate candidates are very low (under 5%).
“Am I too heavy for single-incision?”
Possibly. BMI over 50 makes single-incision technically challenging and may not be safe. During your consultation, I’ll assess your specific anatomy. Some patients with BMI 48 are excellent candidates; some with BMI 42 are not. It depends on fat distribution, torso length, and liver size.
“What about the hernia risk?”
A valid concern. Because the umbilical incision is larger than individual multiport incisions, the theoretical hernia risk could be higher at that single site. However, studies show similar overall port-site hernia rates (around 0.5-2%) for both approaches. My meticulous fascial closure technique addresses this risk specifically.
Frequently Asked Questions (FAQ)
Q: What is single-incision gastric sleeve surgery?
A: Single-incision laparoscopic sleeve gastrectomy (SILSG) is gastric sleeve surgery performed through one 2-3cm incision hidden inside the belly button, rather than the traditional 5-7 incisions across the abdomen. The surgical procedure itself is identical. Only the access method differs, requiring significantly more surgical skill.
Q: How many scars does single-incision gastric sleeve leave?
A: One incision, hidden within the umbilicus (belly button). When fully healed, most patients have no visible scars. The incision is concealed within the natural folds and creases of the navel.
Q: Is single-incision gastric sleeve safer than regular laparoscopic sleeve?
A: Research shows equivalent safety profiles when performed by experienced surgeons. A 2020 meta-analysis of 1,168 patients found no significant differences in complication rates between single-incision and multiport approaches. The key factor is surgeon experience with the technique.
Q: Does single-incision surgery hurt less?
A: Yes. Studies show 30-39% lower pain scores on postoperative days 1 and 2 compared to multiport surgery. Fewer incisions means fewer punctures through abdominal muscles, resulting in less trauma and less pain.
Q: How long does single-incision gastric sleeve surgery take?
A: Approximately 85-100 minutes, compared to 60-90 minutes for standard multiport surgery. The additional time reflects the technical complexity of operating through a single access point. This slight increase in operative time does not affect outcomes.
Q: Who is a good candidate for single-incision gastric sleeve?
A: Ideal candidates have BMI 35-50, no prior upper abdominal surgery, favorable anatomy (xiphoid-to-umbilicus distance <25cm), no large hiatal hernia, and no severe liver enlargement. During consultation, I assess each patient individually.
Q: Who should NOT have single-incision surgery?
A: Patients with BMI >50, previous upper abdominal surgery with likely adhesions, significant liver enlargement, complex hiatal hernia, or very tall stature may be better served by traditional multiport approach. I prioritize safety over cosmetics.
Q: What if the surgeon can’t complete surgery through one incision?
A: Conversion to multiport is always an option and reflects good surgical judgment. If unexpected findings compromise safety, additional ports are added without hesitation. Conversion rates for appropriate candidates are typically under 5%.
Q: Does single-incision surgery cost more?
A: At my practice, no. Single-incision gastric sleeve is included within my standard Enhanced Gastric Sleeve pricing ($5,000-$7,000) for patients who are suitable candidates. This is still a fraction of US surgical costs ($20,000+).
Q: Is single-incision surgery available in Tijuana?
A: Yes, I offer single-incision gastric sleeve at my QUAD A accredited facility in Tijuana, just 20 minutes from the San Diego border. However, not all surgeons in Tijuana have the training or experience to perform this technique safely. Verify credentials carefully.
Q: How do I know if my surgeon is qualified for single-incision surgery?
A: Ask about their specific training in SILS techniques, their case volume for single-incision bariatric procedures, and their conversion rate. Request before-and-after photos showing umbilical scars. A qualified surgeon should be able to answer these questions with specific numbers.
Q: What credentials does Dr. Gabriela have?
A: I am double board-certified (CMCG Mexico, Fellow American College of Surgeons), designated Master Surgeon of Excellence by the Surgical Review Corporation, hold a PhD in molecular biology, and have performed 7,800+ bariatric surgeries. I operate at a QUAD A accredited facility with board-certified MD anesthesiologists exclusively. I’ve been featured in Forbes and Yahoo Finance for patient safety standards. Learn more about my credentials.
The Bottom Line: What Single-Incision Surgery Really Represents
Let me be direct with you.
Single-incision gastric sleeve is not magic. It’s not a different operation. It’s the same Enhanced Gastric Sleeve I’ve perfected over 7,800+ surgeries, accessed through a more technically demanding route.
But the ABILITY to offer single-incision surgery tells you something important about your surgeon.
It tells you they’ve invested in advanced training beyond the minimum required. It tells you they have the manual dexterity to operate in compromised spaces. It tells you they prioritize YOUR experience over their convenience.
When I can safely offer you surgery through a single hidden incision with:
- 30-39% less pain in the critical first 48 hours
- Zero visible scars when healed
- Identical weight loss outcomes
- All the safety features of my Enhanced Protocol
…why would I choose the easier five-port approach?
As I shared in my interview with Forbes, patient outcomes drive every decision I make. Single-incision surgery, for appropriate candidates, simply produces better outcomes on the metrics that matter to patients: pain and cosmetics.
Your Next Step
If you’re considering gastric sleeve surgery and wondering whether single-incision is right for you, here’s what I recommend:
- Check if you qualify eligibility assessment
- Schedule a free virtual consultation where I can review your specific anatomy and medical history
- Ask me directly about single-incision candidacy for your situation
Unlike other clinics, my team includes only board-certified MD anesthesiologists. My facility is QUAD A accredited. My outcomes are audited by the Surgical Review Corporation, which designated me Master Surgeon of Excellence.
I don’t promise single-incision to every patient because not every patient is a candidate. But if you are, I can offer you the most advanced, least invasive approach to weight loss surgery available anywhere.
Five scars or one invisible incision?
When the surgeon has the skills, the choice is yours.